Home Services & Solutions Document process management Essential Preparations: Naviga...
Document Process Management
CIO Bulletin
05 December, 2025
For many people who need a specialized device, the emotional and physical aspects of recovery are challenging enough. Yet, navigating the complex world of insurance and documentation often becomes an unexpected hurdle. Statistics show that a large percentage of initial claims for complex medical devices are initially denied due to missing or inadequate paperwork. This statistic underscores the critical importance of preparedness. You deserve clarity, not confusion, as you pursue independence. This guide will provide the definitive checklist and administrative insights necessary to successfully secure coverage for treatment from a highly-regarded orthotics & prosthetics service near me.
Securing a modern, functional device hinges entirely on establishing medical necessity. This is the core concept an insurance provider uses to determine coverage for a specific device. A device is medically necessary if a physician determines it is required to prevent, diagnose, or treat an illness, injury, condition, or its symptoms, and it meets the standards of good medical practice.
Insurance policies typically categorize prosthetic devices based on function and expected activity level, often known as K-levels. Understanding the expected K-level—whether a person is a non-ambulatory user or someone seeking a running prosthesis—is critical because it dictates what type of componentry the plan will cover. While most major providers in the Southwest cover a foundational prosthetic device, advanced microprocessor knees or feet may require additional justification. Obtaining pre-authorization for high-end prosthetic technology often takes several weeks, emphasizing the need for prompt, accurate initial submission.
Without meticulous documentation, even the strongest case for a specialized solution can be rejected. Insurance companies are not clinicians; they are auditors seeking quantifiable proof that a request meets their strict guidelines. This paperwork trail serves as the necessary evidence. It must logically connect the limb difference or injury to the need for specific prosthetic or orthotic components.
For a new amputee in Las Cruces or an individual seeking an upgrade in El Paso, the initial paperwork is an opportunity to streamline the approval process. Missing a surgical date, omitting a required physician signature, or failing to clearly articulate functional goals can result in frustrating delays. Clear, chronological records significantly accelerate the process and increase approval rates for individuals seeking care across New Mexico and West Texas.
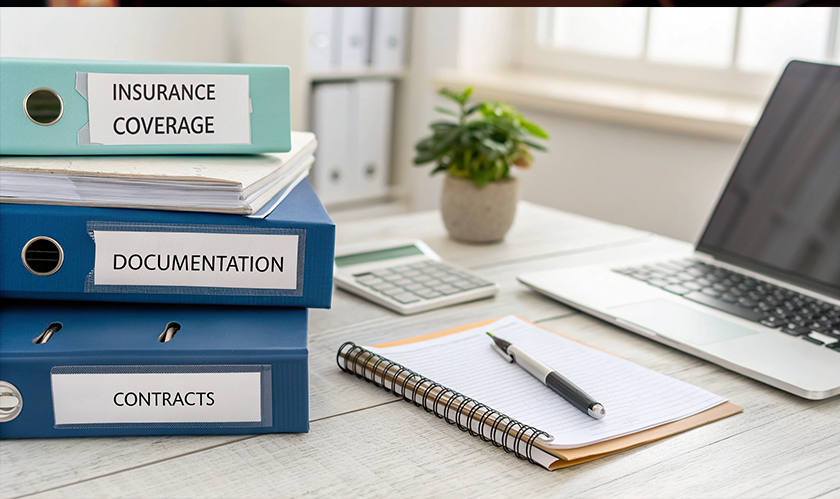
The required paperwork often feels overwhelming, but it falls into two main categories: medical records and administrative forms. Gathering these items correctly is the difference between starting the fitting process promptly and waiting months. Medical records establish the clinical foundation for the claim and must include a formal prescription from the primary care physician or specialist for the specific device, specifying it as a custom solution. Surgical reports detailing the amputation and wound healing status are necessary, along with a Letter of Medical Necessity (LMN). This narrative, written by the doctor, must detail the diagnosis, functional limitations without the device, and specific, measurable goals with the new device. Finally, physical therapy notes, showing current mobility levels and progress, are also required.
Administrative documents confirm identity and eligibility. These include a government-issued photo identification for verification, all current insurance cards (Primary and Secondary), and any past medical records related to the limb loss, including documentation of previous, less expensive devices tried, if applicable. These essential items must be organized and complete.
Once the documentation is complete, the provider manages the submission and follow-up. This process is not a simple transaction; it is a negotiation. First, the LMN and documentation are submitted to the insurance carrier for pre-authorization. A clinical reviewer then compares the documents against the policy's coverage criteria and the provided K-level. If approved, the process proceeds immediately. If the claim is denied, an appeal process begins. This often involves providing additional peer-to-peer discussions or obtaining more detailed clinical notes. Expert administrative management, including specialists who can clearly communicate with patients and family members in both English and Spanish, particularly helps patients in El Paso and Ciudad Juárez.
The price for a custom prosthetic solution is rarely the amount the patient ultimately pays. The final financial responsibility is determined by the policy's fine print, including deductibles, co-pays, and co-insurance. Deductibles are the amount the individual must pay before insurance begins to cover costs. Co-insurance is the individual's percentage share of the allowed charge after the deductible is met. Co-pays are flat fees required for certain services. It is essential to verify these amounts before a fitting begins. Advanced technology is often covered due to proven superior comfort and structural integrity, but it still must go through the proper billing & insurance channels.
Choosing a top clinical provider goes beyond technical expertise; it requires administrative excellence. Individuals must evaluate the provider's ability to manage coverage. When evaluating a provider, patients should ask if they have a dedicated billing and insurance department and if they offer financial counseling to help budget for co-insurance. It is also important to know if they can assist with the appeal process if a claim is denied.
The path to receiving a functional, comfortable custom prosthetic leg involves coordination, expertise, and compassion. While the documentation checklist may seem long, remember that this paperwork represents your future mobility and independence.
By preparing properly, you take control of the administrative requirements, allowing you to focus on your physical recovery and mobility goals.